OpCourage
Combat Stress
Delivering OpCourage services
We are Combat Stress, the UK's leading charity for veterans' mental health
For over a century we’ve been helping former servicemen and women deal with issues like post-traumatic stress disorder (PTSD), anxiety and depression. Today we provide specialist treatment and support for veterans from every service and conflict, focusing on those with complex mental health issues related to their military service.
- Combat Stress is the UK's leading charity for veterans' mental health.
- We provide life-changing treatment and support for veterans from every service and conflict, focusing on those with complex mental health issues.
- Our specialist treatment helps those former servicemen and women with mental health problems such as post-traumatic stress disorder (PTSD), anxiety and depression.
- The complex mental health issues we treat are when someone has several severe mental health conditions arising from military service which often hugely impact on their lives.
- Without our help, lives can become desperate. Anxiety, anger, depression, isolation, alcohol and drug misuse, and in some cases suicide - all can tear families apart, destroy relationships and devastate lives.
- Our aim is to treat veterans' symptoms and improve their quality of life. We want to help veterans tackle their past and take on the future.
- Veterans with complex mental health conditions need a specialist team of different mental health professionals to help them and we provide this. Our clinicians work closely to make a treatment plan for each veteran that is unique to them.
- We have a physical presence in Scotland, England and Northern Ireland. Our treatment is delivered through our treatment centre and treatment hubs as well as online, on the phone and in the community.
- Our vision: We want all former servicemen and women with complex mental health problems to live full and meaningful lives.
- Our mission: To provide support and treatment to veterans with complex mental health problems to help them tackle the past and take on the future.
- We were founded in 1919 in the aftermath of WW1 for veterans with shell shock
- In 1919, the human cost of the First World War was all too obvious. Millions had given their lives during the conflict and thousands returned from the trenches with horrific injuries.
- But not all of the wounds' veterans faced were physical - many who returned struggled to leave the battlefield behind mentally. These servicemen received little or no sympathy from the public. Many were locked away indefinitely in war hospitals and asylums, while others suffered in silence at home.
- But the founders of Combat Stress believed that veterans could be helped to overcome their trauma through rehabilitation.
- Striking out against the contempt and misunderstanding of the era around mental health, Combat Stress began fundraising to introduce residential homes where veterans could live and work, helping them to start rebuilding their lives.
- The treatment for PTSD has changed dramatically over the last century, however the mental health problems that former servicemen and women can face are as relevant as ever.
- For over century now, Combat Stress has been helping former servicemen and women deal with issues like post-traumatic stress disorder (PTSD), anxiety and depression.
We are the UK's leading veterans' mental health charity because:
- No other charity in the UK does what we do. We provide the only intensive mental health treatment service to veterans in the UK. Our services are veteran-focused, designed to treat veterans' symptoms and improve their quality of life.
- Our services are delivered by our own specialist clinical teams across various disciplines to provide a care package for each veteran based on their individual needs.
- Our team is experienced at producing world-leading clinical outcomes.
- All employees are trained to understand trauma and its impact so that every interaction with the charity contributes positively to the veteran's recovery.
- Our services in the UK have a regulator rating of Good (Care Quality Commission - England) or Very Good (Care Inspectorate - Scotland).
- We are the Strategic Lead for the Clinical Quality in Mental Health (funded by the Armed Forces Covenant Fund). We provide training to other organisations on how to work with the NHS, how to achieve the quality kitemark set by Cobseo and the Contact Group, understanding the veteran community, mental health first aid and understanding mental health conditions. By helping with training in all these organisations, our aim is to reduce suicide rates amongst veterans.
- We have a highly productive and influential research department and continue to explore innovative and effective ways of treating veterans and their families.
We are pleased to partner with a number of NHS providers to deliver elements of both the Complex Treatment Service (CTS) and High-Intensity Service (HIS) across the UK. Combat Stress provides the expertise required to deliver the services.

NHS England High-Intensity Service (HIS) for veterans in the north of England.
- Out of hours Clinician-led advice line
- Research and evaluation
- Family Peer Mentors
NHS Complex Treatment Service (CTS) across the north of England
- Peer support services
- Substance misuse nursing
- Addiction Support Workers
NHS High-Intensity Service (HIS) across the Southwest of England
- Out of hours Clinician Advice Line
- Specialist clinical training
- Psychology services and training
- Mentorship
OUR MILITARY MIND SYMPOSIUM
Innovations and collaboration for the care of veterans
In May 2022, we were honoured to have some eminent speakers, including Professor Sir Simon Wessely and Kate Davies, NHS England's Director of Health and Justice, Armed Forces Health and Sexual Assault Services, present alongside senior members of the Combat Stress team at our Military Mind Symposium. The event included updates on key services at Combat Stress, insights into areas for further exploration and innovation and an overview of existing and planned collaboration to improve access to mental health services for veterans.
To watch the symposium, please visit: https://youtu.be/l8St13Yyoiw
- Registered with Care Quality Commission in England, with 'good' ratings
- Registered with Care Inspectorate in Scotland, with 'good' and 'very good' ratings
- Registered with the Regulation & Quality Improvement Authority (RQIA) in Northern Ireland. RQIA were satisfied with the inspection in October 2021 and did not identify any areas for improvement - testament to the staff adherence and compliance with standards.
- A participant in the Royal College of Psychiatrists Quality Network for Veterans' Mental Health Services Peer Review
- A finalist in the 2021 Royal College of Psychiatrists Team of the Year Award
- A finalist in the 2021 Health Service Journal Military and Civilian Health Partnership Award
- A member of the Confederation of Service Charities
- A member of the Contact Group
- A member of the Five Eyes international research collaboration
- An internationally renowned research team
- In a partnership with Virginia Mason Institute (Seattle, USA) to deliver Combat Stress' continuous improvement strategy

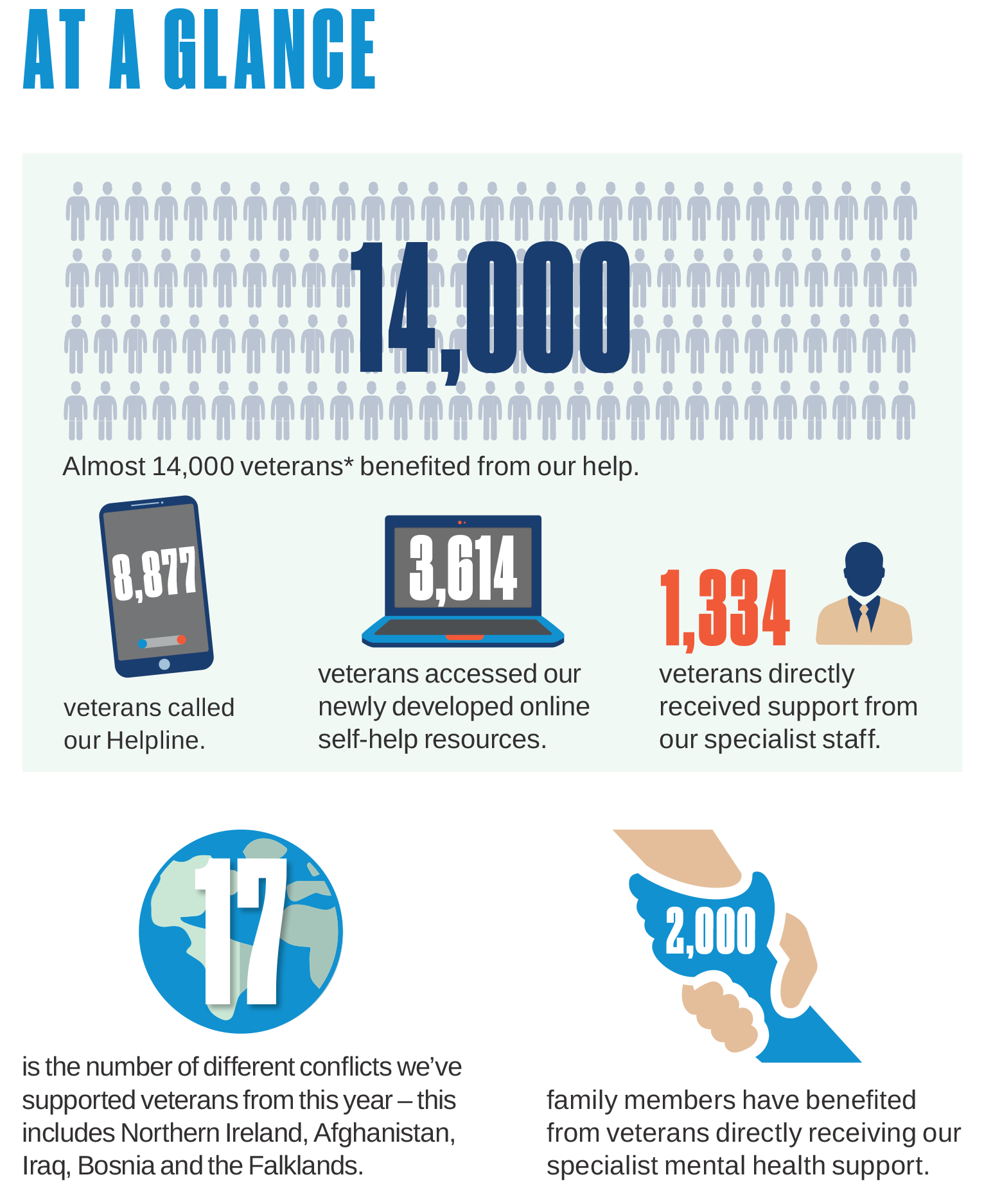
Our 24-hour Helpline is the first step on a veteran's journey. The Helpline is staffed by a team of highly skilled and compassionate call handlers who will help veterans to complete a referral form online. After the assessment, we work with the veteran to plan their treatment to best suit their needs.
There are four areas of treatment available, and each treatment plan is unique to each veteran. A veteran's treatment may comprise one or more of the following areas of help:
Building Resilience
Treatments here give veterans tools to enable them to manage their mental health better and improve the quality of their life. Veterans receive help to build a 'toolkit' of skills and resources that they can use in their day-to-day life so they can manage better. For example, learn ways to reduce the amount they drink; have help to feel less anxious or low in mood; find ways to stop trauma memories interrupting daily life, or manage nightmares affecting their sleep. Treatments here are normally delivered in groups by Nurses, Occupational Therapists, and Family Support Workers. We also offer a programme that supports partners of veterans to better understand veterans' mental health problems and how to take care of themselves as they support their veteran partner's recovery.
Managing the Consequences of Trauma
Treatments here are for some of the more complex difficulties that veterans may be having following traumatic experiences. They may have help to feel better about themselves, particularly if they struggle with guilt or shame about their past. Other help includes support for veterans to understand and manage overwhelming emotions, such as anger or fear, or conversely to help when they feel 'cut-off' from their emotions. A further type of help is for veterans who want to be able to manage relationships better. Art Therapists also work with veterans who need help to step into trauma-focused treatment, and to feel more confident about doing so. All of these treatments are delivered in groups by our psychological therapists. Some individual treatment is also available to veterans who need it —Psychiatrists offer specialist medical consultation, advice and treatment, whilst Occupational Therapists can also offer individual treatment about transition, identity and occupational function
Trauma-focused Treatment
This involves specialist treatment called trauma-focused psychological therapy. This involves Psychological Therapists working with individual Veterans. Therapy involves talking about traumatic experiences in a way that is manageable for the veteran. This can effectively change the way traumatic memories are stored in the brain and reduce many symptoms of Post-Traumatic Stress Disorder and Complex Post-Traumatic Stress Disorder. Alternatively, some veterans may find it easier to 're-visit' traumatic memories using Art Therapy; an approach that is less reliant on verbal processes, and which is available to those who need it.
Looking to the Future
This is where we help veterans to invest in meaningful roles and activities that are important to them, including relationships, leisure, work, life situations and the communities where they live. This is an important part of recovery and this part of the service is led by our Occupational Therapists.
As well as the clinical treatments briefly described above, we have other parts of our service that support veterans and their families into, through and beyond treatment including peer recovery workers, our peer support service and our family support service.
We also have accessible online help and advice for veterans on our website that is evidence-based and of high clinical quality. Veterans can watch our clinicians talk about mental health difficulties that might affect them and read information about what to do to help themselves. There is also help and advice for veterans' families, employers and other organisations who support veterans. These materials enable veterans to start to understand their difficulties even before contacting us for help and can continue to be used during treatment and afterwards. Veterans with needs for which we do not have a suitable service can also benefit from accessing these materials.
- Our research team is part of national and international projects contributing to research in veterans' mental health and innovations in treatment. Our clinicians use this to continually improve the effectiveness of our service and ensure we are delivering evidence-based treatments.
- Our research department was established in 2014 and is led by Prof Dominic Murphy. We are committed to publishing our research in external peer-reviewed academic journals as part of our commitment to contribute to the advancement of the veteran mental health field. We recently published our 100th paper
- Professor Murphy is a member of the Kings Centre for Military Health research at Kings College London. Our research department operates between the two organisations to ensure our research is of the highest standards.
- Our research team investigates veterans' mental health needs, evaluates treatment outcomes and develops clinical services based on research findings.
- Along with our Five Eyes allies in the US, Canada, New Zealand and Australia, Combat Stress is a world leader in veterans' mental health, at the forefront of developing, assessing, and introducing new and improved diagnoses and treatment of veterans' complex trauma-related mental health needs.
View our research library.
Chloe Mackay CEO, Combat Stress

Chloe is responsible for the veterans’ services of the Forces Employment Charity, including employment programmes for ex-Forces, spouses and partners of veterans, and still-serving personnel. She also has responsibility for our support to veterans in the criminal justice system and Chairs the Cobseo Justice Cluster. Chloe joined the organisation in 2016 from the cancer charity sector following roles as Head of Strategy at Macmillan and Breast Cancer Now.
Before working in the charity sector, she was a management consultant and worked for ten years for PricewaterhouseCoopers and IBM.
Dr Naomi Wilson, Clinical Director, Combat Stress

Dr Naomi Wilson is Clinical Director for Combat Stress. She is an expert in the provision of psychological therapy for complex trauma-related mental health difficulties.
She is passionate about improving therapeutic effectiveness in treatments for post-traumatic mental health issues, understanding what works at both an individual and system level, and building mental health services that are trauma-informed where both the client group and staff can thrive.
Naomi has recently led the transformation of Combat Stress's clinical services so that veterans can access the highest quality, evidence-based, accessible treatments (all of which were delivered online during COVID19) within a framework that attends to the familial and support systems important to veterans are living; to maximise recovery and ameliorate the potential for intergenerational trauma.
Naomi has extensive clinical supervision, teaching, training and research experience in trauma-related mental health difficulties, particularly 'Complex-PTSD' in individuals who have experienced multiple traumas across their lifetime. She was an elected Board member of the UK Psychological Trauma Society until 2020 and has held academic posts at the University of Sheffield and University of Surrey in Clinical Psychology doctoral training programmes.
Naomi works closely with the Head of Research, Prof Dominic Murphy, to evaluate the services within Combat Stress, and research and implement treatment innovations that aim to contribute to the advancement of the veteran mental health field.
Professor Dominic Murphy, Head of Research, Combat Stress

Dominic gained his first degree, an MA in psychology from Glasgow University in 2003. He then joined King's College London as part of the team that established the King's Centre for Military Health Research (KCMHR) and setup an ongoing UK military study following the 2003 Iraq War.
Dominic earned his doctorate at KCL exploring vaccinations and medically unexplained symptoms in military personnel in 2010. Dominic then trained as a Clinical Psychologist and completed his clinical doctorate at Royal Holloway University in 2013.
In 2013, Dominic joined Combat Stress (a national veterans mental health charity in the UK) where he established and now leads a research department specialising in veteran's mental health.
The Combat Stress research department is co-located within the KCMHR where Dominic continues to be a member. Dominic is part of the Five Eyes Veterans Mental Health Consortium, a Director and Trustee for the Forces in Mind Trust, works on NATO research task groups, been a special editor for a number of journals and member of several international military mental health research consortiums and scientific advisory boards. In 2019, he was elected the President of the UK Psychological Trauma Society (UKPTS) and onto the executive board of the European Society for Traumatic Stress Studies (ESTSS).
Dominic has specialised clinically and academically within the field of PTSD and military mental health and is widely published with over 140 articles to date. Currently Dominic is leading a number of clinical trials. These include an RCT exploring the efficacy of a novel modular treatment for Complex PTSD, an RCT exploring the impact of an App to reduce drinking in veterans with a dual diagnosis and a feasibility trial to develop and new intervention to treatment Moral Injury.
Our research has included:
To find out more about our research visit www.combatstress.org.uk/research
NHS Armed Forces Team
"NHS England has worked closely with Combat Stress since 2013, during which time it has witnessed its impressive growth and development, no more so than during the COVID-19 pandemic. Throughout this turbulent period, the charity was pivotal in adapting working practices to ensure the ongoing provision of mental health support for veterans. The vital work carried out by charities working in this area, together with the NHS, is of growing importance in driving improvements in mental health and wellbeing outcomes for veterans and their families, which Combat Stress is very much at the forefront of championing."
Leeds and York NHS Partnership Trust
"Leeds and York Partnership NHS Foundation Trust has worked closely with Combat Stress since 2018, during which time the two organisations have forged a strong working relationship. Combat Stress is an important partner in the delivery of the Veterans Mental Health Service (OpCourage) and remains in close collaboration with Leeds and York through this next stage of the OpCourage contract. The vital work carried out by Combat Stress in this area, together with the NHS, is of growing importance in driving the continuous improvements in mental health and wellbeing outcomes for veterans and their families."
