Living with Chronic Pain
Are you struggling with chronic pain?
Many veterans struggle with chronic pain and frequently have other physical or psychological complications alongside their pain. You may find this is more intense currently due to the impact of the COVID-19 virus on our daily lives.
This page will discuss how we might better understand the components of chronic pain (biological, psychological, and emotional). It will also offer you ideas on how you might manage more effectively, particularly where you may feel more vulnerable / less able to cope given the necessary restrictions placed upon us during COVID-19.
What is ‘Chronic Pain’?
Chronic pain refers to pain with a duration of three months or greater that is often associated with functional, psychological and social problems that can negatively impact a person’s life
It is important to note that some people’s chronic pain stems from a traumatic event. In these cases, the chronic pain itself may actually serve as a reminder of the traumatic event, which will often make a veteran’s psychological symptoms even worse.
Other examples of common psychological difficulties resulting from chronic pain amongst veterans include the following:
- Insomnia or lack of sleep
- Anxiety about current and potential discomfort
- Feeling low in mood or that life is not worth living
- Memory and/or cognitive issues (e.g. concentration or attention problems)
- Anger/ irritability/ isolation/social withdrawal which may be exacerbated by the lockdown measures
- Problems maintaining relationships
If you are struggling with any of these issues, please do refer to the other Combat StressCOVID-19 resources
Here are some short video clips you may find helpful:
- Understanding Pain What to do about it - 5 min clip
- How does your brain respond to pain? - 5 min clip
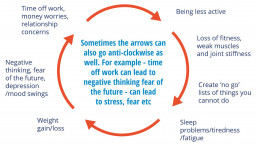
The Persistent Pain Cycle
Because chronic pain is very complex—it includes biological, psychological, and emotional components - all of these factors must be managed to treat your pain effectively. Take a look at the persistent pain cycle below, do any of these experiences sound familiar to you?
How do I Manage Pain?
If you have been living with pain for a long time, you may find it affects your life in a lot of different ways
Some common difficulties are:
- Not being able to continue with hobbies and sport
- Feeling stiffer and weaker
- Not wanting to take part in social activities
- Finding it difficult to deal with increases in pain or flare-ups
- Difficulties sleeping or sleeping too much
- Worrying about pain or the future
- Loss of self-confidence and feeling low
- Not being able to explain pain to others or feeling that others don’t understand
Here are some ideas of ways to manage your pain:
1. Keeping active
Gentle exercise is an important part of managing pain. Please check with your GP before commencing exercise if you are restarting exercise after a long break. Some people worry that if they exercise, they will make their condition worse. Research shows that gentle exercise is good for people with chronic pain because it:
- improves strength, stamina and flexibility /improves your overall health
- can benefit your emotional health /releases endorphins (natural pain killers) into the system.
- helps with balance and coordination /helps improve sleep
- helps with joint health - our bodies were designed to move.
- The best form of exercise is usually the one you enjoy most. This is because you are more likely to stick with it.
2. Pacing
Chronic pain can make it difficult to remain active. You might try and push yourself to do as much as you can on good days. This can cause an increase in pain, so that you need to reduce your activity for a few days. This is sometimes called a ‘boom and bust’ pattern. It can lead to reduced activity over time.
Pacing is a key skill in pain management. It involves taking a break before you need to, so you have a consistent pattern of activity and rest. Over time, this is associated with being able to do more.
Often the veterans we work with tell us they are surprised how much they can get done by sticking to this approach.
3. Managing thoughts and feelings
Pain can be stressful and upsetting to deal with. You may find that pain affects your work, hobbies, social lives and relationships. If pain carries on for a while it can lead to you feeling worried, frustrated or low.
Difficult thoughts and feelings are an understandable and normal reaction to pain. Low mood and anxiety can make the pain system more sensitive. They can make pain worse or make it harder to cope with. People who find ways to manage their thoughts and feelings often feel more confident in managing their pain, feel less down and find that their pain gets in the way of life less.
4. Managing flare-ups of pain
People with long term pain often have times when their pain increases significantly, and they are able to do less. These are often called flare-ups and usually last for a few hours to a few days. Flare-ups are a difficult but normal part of living with chronic pain.
If you have not been given specific advice on flare-up management, some of the ideas here may help:
- Balance rest with gentle movement. Moving regularly is good for joints and muscles and can reduce or prevent stiffness.
- Take your medication as prescribed.
- Remind yourself of how you coped before. Some people find it helpful to remind themselves that flare-ups don’t mean there is any new damage to their bodies. Reminding yourself that it will pass can also help.
- Relaxation can help reduce muscle tension - It can be beneficial physically and psychologically – important to practice when feeling less unwell.
Special note about COVID-10 and the use of Ibuprofen and other non steroidal anti-inflammatory drugs:
You may be aware of issues currently being investigated with regard to the use of Ibuprofen and other non-steroidal anti-inflammatory drugs (NSAIDs) for managing fever and pain in people with suspected COVID-19:
Information from the British Pain Society: Ibuprofen and COVID-19
At the present time there is currently no strong evidence confirming that ibuprofen increases the likelihood of contracting the virus or worsening the symptoms; however, its anti-inflammatory and anti-pyretic effects may mask the symptoms and signs of COVID-19 infection. The MHRA and NICE are reviewing the evidence urgently. At present, patients who have confirmed COVID-19 infection, or believe they have COVID-19 infection, should take paracetamol in preference to ibuprofen.
If you have been prescribed ibuprofen, non steroidal anti inflammatory drugs (NSAIDs) or any other medicine and are taking them regularly you should not stop without taking advice from a GP/Pain specialist
Keep the use of all analgesics to a minimum because these can, in fact, make certain pain worse if overused.
Recommended Resources
- Struggling to be me with chronic pain (Youtube video clip)
- The Pain Toolkit - general tips on living with long term pain
- The British Pain Society
- Relaxation & Mindfulness
Is there someone I can call and talk to?
Our 24/7 free Helpline remains open, so please do not hesitate to call if you need someone to talk to or any guidance during this difficult time.
Combat Stress 24/7 Free Helpline 0800 138 1619.

